Glue ear and hearing loss in children
Details of the condition
GLUE EAR AND MIDDLE EAR INFECTIONS
- Glue ear and recurrent acute otitis media are part of the same spectrum of suppurative otitis media, and as such are considered together.
- It is possible for the presenting complaint to be with glue ear (hearing loss) or recurrent ear infections (pain/ fever) by themselves, or these problems can occur together.
- When the symptoms are severe and persistent over a prolonged period for any of these clinical scenarios, grommet insertion becomes an option.
WHERE IS YOUR MIDDLE EAR?
- The middle ear is normally an air-filled space between the ear drum and the inner ear (cochlea).
- It contains the bones of hearing which connect the ear drum to the inner ear.
- Infections enter the middle ear form the back of the nose via the eustachian tube, causing pain, fever and loss of hearing. The ear fills with pus.
- If the eustachian tube is blocked over a prolonged period, the middle ear fills with thick mucus (“glue ear”) causing hearing loss, because the ear drum cannot vibrate properly
WHAT IS MIDDLE EAR INFECTION?
- Acute otitis media is a painful infection of the ear which is common in young children.
- It usually follows a viral infection, and probably relates to secondary infection from bacteria including Streptococus pnumoniae, and Haemophilus influenzae.
- A few middle ear infections per year may be part of normal development, and are usually treated with antibiotics.
- If infections are too frequent, then grommet insertion is likely to help the situation.
WHAT IS THE DIFFERENCE BETWEEN A MIDDLE EAR INFECTION AND GLUE EAR?
- A middle ear infection – is associated with significant pain, fever and an unwell child. It represents an abscess (pus) behind the eardrum.
- Glue ear – can occur after an infection, or can occur without a clear history of ear infection. It thick mucus, or golden fluid behind the ear drum It is not painful, and the child is well. It is associated with hearing loss.
WHEN DO MIDDLE EAR INFECTIONS OCCUR?
- Middle ear problems are experienced at some stage by majority of children.
- There is a natural fluctuation of middle ear issues, related to the seasons, and an improvement with age (seen between 4-6 for most children).
HOW DO EAR INFECTIONS AFFECT YOUR HEALTH?
- Too many infections leave a child constantly having fevers, being run down, sleeping poorly and requiring multiple trips to the doctors and courses of antibiotics.
- Ear infections are very disruptive to lives of children and their families who often have to take a lot of time out of their routine schedule, with time off kindy, school or work.
SYMPTOMS OF MIDDLE EAR INFECTIONS?
- Pain
- Fever
- Reduced hearing
WHAT ARE THE BEHAVIOURAL INDICATIONS OF EAR INFECTION?
- Ear symptoms can vary with age but behaviour associated with a painful middle ear in a young child can include:
- Abnormal irritability
- Feeding difficulties
- Consistent presence of fever
- Ear tugging
- Disturbed sleep.
- A miserable and unwell child
HEARING LOSS SYMPTOMS ASSOCIATED WITH MIDDLE EAR INFECTION
- Typically, glue ear will present as a mild-to-moderate hearing loss, similar to walking around with your fingers blocking your ears.
- The best possible hearing in children is often substantially better than what is considered “normal“ in the adult population. This mean there is a degree of reserve.
- A child’s hearing will typically still hear one-on-one but will struggle in more challenging auditory environments.
- In many cases, the hearing loss is very obvious to parents, carers and teachers.
WHAT ARE THE STAGES OF A MIDDLE EAR INFECTION?
- The first stage is pain and fever
- The acute infection may:
- Resolve spontaneously with time, with the ear returning to normal.
- Resolve with the help of antibiotics
- Burst the ear drum with pus discharge from the ear. In most cases the pain will then improve, and the hole in the ear drum will heal.
- The infection may settle, but the patient is left with glue ear (thick mucus behind the ear drum), which causes hearing loss.
WHAT ARE THE CONSEQUENCES IF UNTREATED EAR INFECTION?
- In rare cases where no action is taken there may be severe complications including meningitis and brain abscess.
- There may be permanent structural damage to the ear drum if multiple recurrent ear infections occur without appropriate treatment.
- If infections are too frequent or too severe, antibiotics are no longer enough and grommets will be required to improve the child’s wellbeing.
WHAT ARE THE CAUSES OF MIDDLE EAR INFECTIONS
- Children have immature eustachian tubes and immune systems leaving them more susceptible to the upper respiratory infections which we all encounter through the year.
- This sets the scene for a secondary infection with nasty bacteria (eg Streptococci, Haemophilus) which cause ear infections.
- Children become less prone to infections once they reach school age (4-6).
- For the worst cases ear infections may continue beyond this age group.
MY CHILD GETS A LOT OF EAR INFECTIONS. HOW MANY EAR INFECTIONS ARE TOO MANY?
- Most young children will have ear infections from time to time. This is more common when they are in kindergarten or day care, and over the winter months.
- Once the infections are “back to back”, with frequent antibiotics and visits to the local doctor consideration should be given to a specialist ENT referral.
- There may be associated hearing loss with glue ear, and part of the assessment will probably include a hearing test.
- In the circumstance of severe recurrent ear infections, grommet insertion can dramatically improve your child’s quality of life and substantially reduce the requirement for antibiotics.
HOW DO THE MIDDLE EAR INFECTIONS AFFECT YOUR CHILD’S HEALTH?
- Impact from Middle Ear Infection can include:
- Delay in educational development.
- Frequent middle ear infections cause ongoing misery for a child and their family.
- Lifelong problems caused by hearing loss.
WHY HAS A HEARING TEST BEEN RECOMMENDED?
- Hearing testing is routine in children with suspected middle ear problems, and helps to predict which children would be helped by an operation.
- Various hearing tests can determine if there is hearing loss at a level that will compromise a child’s educational development.
DIAGNOSIS OF MIDDLE EAR DISEASE
-
- Middle ear disease can be diagnosed by your doctor when the history is taken. Middle ear disease is indicated when a child presents with:
- ear pain
- fever
- unsettled child, poor sleep
- deafness
- language delay
- other ENT symptoms such as blocked nose, thick snot, cough , tonsillitis, snoring
During an examination your doctor will possibly see:
● characteristic red, swollen ear drum in middle ear infections (below)

Figure: the red drum of acute otitis media
- golden or dull ear drum with fluid

Figure: the golden drum of glue ear
- Middle ear disease can be diagnosed by your doctor when the history is taken. Middle ear disease is indicated when a child presents with:
TESTING THE EAR WITH MIDDLE EAR INFECTION OR MIDDLE EAR FLUID
TYMPANOMETRY
- Tympanometry tests the condition and function of the middle ear. It is not a hearing test.
- It measures the energy transmitted through the eardrum (tympanic membrane) to the conduction bones by creating variations of air pressure in the ear canal.
- The test assesses the presence of abnormal pressure behind the eardrum.
- Tympanometry is helpful in making the diagnosis of middle ear fluid build up (effusion).
- It is a useful screen for children who may have hearing loss.
AUDIOMETRY
-
- Visually reinforced audiology
- Audiometry is a test to determine hearing levels or hearing loss. The test It will normally take 15 minutes to half an hour.
- We use distraction devices like the dancing puppet which makes the hearing test an enjoyable game for young children.
- Paediatric Visual Reinforcement Audiometry (VRA), or the Puppet Show Test is used with infants from 6 months up to children of 2 years.
- The puppet makes the hearing test like a game. The puppet will do an amusing dance if the child responds to a sound stimulus correctly.
- VRA is in a sound field meaning it tests the overall function of both ears together, rather than each ear separately.
Figure: The puppet-show, used in sound field testing for young children (typically 6-24 months)
- Ear specific audiology
- In children older than 2 years, it is usually possible to test the ears individually.
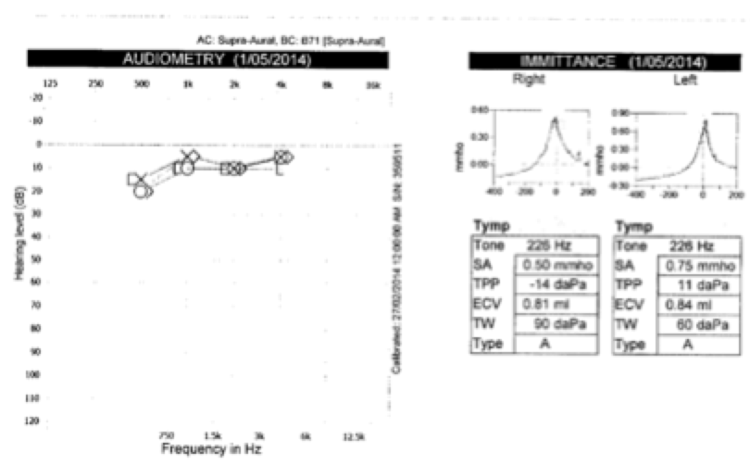
Figure: a hearing test of both ears confirming normal midle ear function and hearing in both ears for a 3 year old
- Otoacoustic emissions
- This provides a pass/ fail test of overall ear function, and can be useful in very young children.
- A pass gives reassurance about normal middle and inner ear function.
- A fail is most commonly related to middle ear fluid
- Visually reinforced audiology
TREATMENTS FOR MIDDLE EAR INFECTIONS
- When patients present with persistent fluid or recurrent Middle Ear Infections there are a number of common courses of action. These are typically either:
- Watchful Waiting
- valsalva- eg EarPopper device
- Allergy treatment (spray such as nasonex)
- Long term, low dose antibiotics
- Grommet insertion
- When there is a history of multiple ear infections or persistent middle ear fluid with hearing loss, it is likely that an Ear, Nose and Throat (ENT) specialist will be involved in care.
WATCHFUL WAITING FOR RECURRING MIDDLE EAR INFECTION
- Usually middle ear infections are self-limiting and may require nothing more than clinical monitoring or the occasional course of antibiotics.
- The “wait and see” approach in some cases is advised. This approach acknowledges both the seasonal fluctuation in symptoms, and that most children have less symptoms as they get older.
- Improvement in middle ear infections normally, but not always, commences in the 4-6 year old age group.
ALTERNATE APPROACHES FOR MIDDLE EAR INFECTIONS
- There is no good evidence for any treatment other than grommets for persistent Middle Ear Infections, but other treatments are:
- Nasal Allergy Treatment may have some benefit, when allergic rhinitis is an issue in its own right. Using nasal sprays such as Nasonex may have a role.
- Inflation of the middle ear
- Using an EarPopper has some evidence for efficacy but can be difficult for children to tolerate.
- It is a device that pumps pressure into the Eustachian tube via the nose has some evidence, especially in adults but is not tolerated by many young children.
- Antibiotic Therapy – Long-term antibiotics have limited evidence, and carry potential issues with side effects and antibiotic resistance.
GROMMETS
WHAT ARE GROMMETS?
- Grommets are the surgical implant of a tube in the eardrum to drain fluid from the middle ear.
- At the time that grommets are inserted, any fluid present behind the eardrum is removed with a microscopic suction tube.
- Grommets are tiny ventilation tubes that are place through the eardrum like a button. They are designed to correct abnormal pressure behind the eardrum.

Figure: grommets of various sizes and designs. The white grommet at the top right is a Sheehy fluoroplastic collar button tube, the grommet most commonly used by Dr Smith.
Figure (below)- gives an idea of the shape and size of typical grommets (Scale in cm)
WHEN TO CONSIDER GROMMETS
- Grommets are a very effective treatment when there is evidence of persistent abnormality of the middle ear, either with persistent hearing loss or where there are too many infections, and “too many antibiotics”.
- Evidence shows Grommets are the best treatment to help children with overly frequent middle ear infection or fluid with hearing loss.
- Grommets will be considered with hearing loss of both ears (normally more than 3 months), particularly if there is concern with language development.
- Grommets may be considered if there are more than 6 episodes of acute otitis media in a 12-month period, or 3-4 infections a year, for multiple years. The threshold to intervene may be lowered if there is associated hearing loss. Ultimately, the point of intervention is when the occurrence of ear infections becomes an almost constant ongoing stress for the child and their family.
HOW GROMMETS BENEFITS YOU
- For children who struggle with their ear problems, in most cases Grommet will:
- Dramatically curb the number of ear infections
- Almost immediately improve hearing to normal
- Improve the wellbeing and the quality of a child’s life.
- If your child does contract an ear infection the pain would be greatly reduced and manifest as a simple discharge, rather than pain and fever.
WHAT ARE THE CONSEQUENCES UNTREATED MIDDLE EAR DISEASE?
- Consequence on inaction are:
- Delay in educational development.
- Lifelong problems are also cause if hearing loss is ignored for a long time
- Overly frequent middle ear infections cause ongoing misery in the lives of a child and their family.
- Use of too many antibiotics can cause upset stomachs
- Dependence on antibiotics can increase the build up antibiotic resistance which may ultimately result in loss of efficacy.
- Rarely, there can be a life-threatening complication of middle ear infection (eg meningtis, brain abscess)
- Where Grommets are indicated there are theoretical risks if you elect against the procedure
- Long term structural change to the eardrum may require surgery in adulthood.
- Persistent hearing loss
- Irreversible hearing loss.
- There is a very small chance of a major complication of ongoing middle ear infections, including meningitis, and cerebral abscess.
INVESTIGATION BEFORE GROMMET INSERTION
- An audiogram is routinely obtained prior to grommet insertion.
GROMMET SURGERY
- Grommet implant surgery requires a general anaesthetic in one of the local hospital and is a day-only procedure.
- It is a very simple procedure with very pleasing results. We usually expect a dramatic improvement in hearing, ear infections or both.
- Even if there are ear infections after grommet insertion, they are usually much less severe.
- Your child will be back to normal activities by the next day in most cases.
- When grommet surgery is performed as a stand alone procedure, the only downtime is the day of surgery. If it is combined with other procedures (eg tonsillectomy), more time off will be required.
PREPARATION FOR SURGERY
- The hospital will be in touch the day prior to surgery to confirm fasting information, where to park, how to get to the appropriate part of the hospital, what time to turn up and what to bring/ wear bracket omitted here.
AFTER GROMMET SURGERY CARE
- There is minimal pain postoperatively, and the child is usually discharged several hours after the procedure.
- Hearing improvement will often be noticed immediately
- Ciloxan ear drops will be used to both ears for 5 days.
- The first review appointment is at about 2 weeks.
- The ears should be kept dry for the first 2 weeks.
- Earplugs are not necessary in the first couple of weeks but will be discussed at the first postoperative review with a view to returning to full water activities.
WATER PRECAUTIONS AFTER SURGERY
- Until the post operative review 2 weeks after the Grommet procedure the ears should be kept dry. This means:
- No Submerging the head in bathwater.
- Hair washing is not a problem if the hair is rinsed with fresh water from the tap or a shower.
- Swimming should be avoided until the first postoperative review.
DOES MY CHILD NEED EAR PLUGS AFTER GROMMET SURGERY?
-
- With or without ear protection, infections are still possible.
- There is controversy about earplug usage between ENT surgeons, but most who are located in areas where there is a high frequency of swimming and other water sports recommend their use.
- If ear plugs are well-tolerated, Dr Smith recommends their use when swimming. The ear plugs should be reinforced with a headband, or swimming cap.
- At bath time, plugs are not necessary, but it is important that the head not be put under the water in the bath, and that the hair is rinsed with fresh water from the tap or shower.
- There are different options are available for ear plugs:
(1) Blu Tack is favoured by many parents, and with good reason. It is easy to use, cheap and replaceable. The Blu Tack should be moulded to fill the bowl of the ear, with a tail into the outside part of the ear canal.
(2) Doc’s Proplugs is a good solution for some kids. A size can be found to fit most kids. They stay in the ear well, in many cases.
(3) Custom ear plugs (GN Resound) may be superior in some (but not all) patients.
- Doc’s Proplugs, custom plugs and neoprene headbands for children are all available through our audiology service, both in the Miranda and Annandale offices.
WHAT IS THE POST SURGERY FOLLOW UP SCHEDULE AFTER GROMMET INSERTION?
After Grommet surgery Dr Smith recommends the following schedule:
-
-
- Two Weeks are surgery
- Every 6 months until the grommets have come out.
- In the event of discharge (mucky fluid coming out of the ear), more frequent review may be necessary.
- These appointments usually last for 1-2 years.
- The most common pathway is that the ears remain relatively problem free for the life span of the grommets.
-
HOW LONG DO GROMMETS LAST? DO GROMMETS FALL OUT BY THEMSELVES OR DO THEY NEED TO BE REMOVED?
- The grommets, on average, will last between 12 and 24 months. When they come out, the child’s ears have often returned to normal.
- In most cases, the Grommets come out by themselves and the eardrum heals.
- Often, at this stage, the ear will have returned to normal.
- In some cases, another set of grommets may be required or surgery may be required to fix a persistent hole in the ear drum.
- Occasionally, a grommet will need to be removed when it has been in the ear for too long (>3 years).
- The grommet may need to be removed if it causes problems such as uncontrolled discharge from the ear.
- The grommet can also come out early <6 months (in rare cases) If there are still middle ear issues at this stage, a further set of grommets may be required.
POST SURGICAL ISSUES AFTER GROMMETS
THERE IS THICK FLUID/ MUCUS COMING OUT OF MY CHILD'S EAR AFTER GROMMET SURGERY? IS THIS NORMAL?
- The most common post-surgical issue is discharge from the grommet. (Pus coming from the ear)
- IT IS IMPORTANT TO RECOGNISE THAT DISCHARGE IS NOT A NORMAL PART OF “THE GROMMET DOING ITS JOB”.
- WE DON’T EXPECT DISCHARGE FROM THE EAR WHILE THE GROMMET IS IN PLACE.
- If there is discharge, there is an infection which should be treated with Ciloxan ear drops in most cases (not oral antibiotics such as amoxyl).
- Your GP may be happy to treat this, but we would appreciate a phone call to let us know what is happening.
- If there is any issue we are very happy to see your child at short notice to ensure the infection settles.
POST OPERATIVE INFECTIONS
- Ongoing ear infections may arise from water that has gone through the grommet from the outside and stagnates.
- It is overall more common in summer months, associated with greater time in the water.
- The mainstay of treatment is antibiotic ear drops (usually Ciloxan) guided by swab results.
- The ear may need to be cleaned with suction, under microscopic vision.
- The grommet may also discharge after an upper respiratory infection, and there may be similar bacteria to acute otitis media in the child without grommets (e.g. Streptococcus, Haemophilus).
- Ear drops will still be effective in majority of cases, but antibiotics by mouth sometimes have a role, as guided by microbiology swab results.
IF APPROPRIATE TREATMENT IS NOT UNDERTAKEN PROMPTLY, IT:
- Increases the chance that a persistent infection of the grommet becomes established
- In the worst cases, may require the grommet to be removed with another operation.
REVISION (REPEAT) GROMMET SURGERY
Another operation is required down the track. Reasons for this include:
- to remove a grommet that has stayed in for too long
- to remove a grommet that has too many episodes of infection/discharge
- to repair a small hole that is left behind after the grommet has come out
- to insert another set of grommets if the child develops recurrent infections, or middle ear fluid with hearing loss after the previous set of grommets has come out.



